A Response to the University of Illinois’ Explanation of Its False Saliva-Test Claim
An article I posted on Twitter via Google Docs on 10/13/20
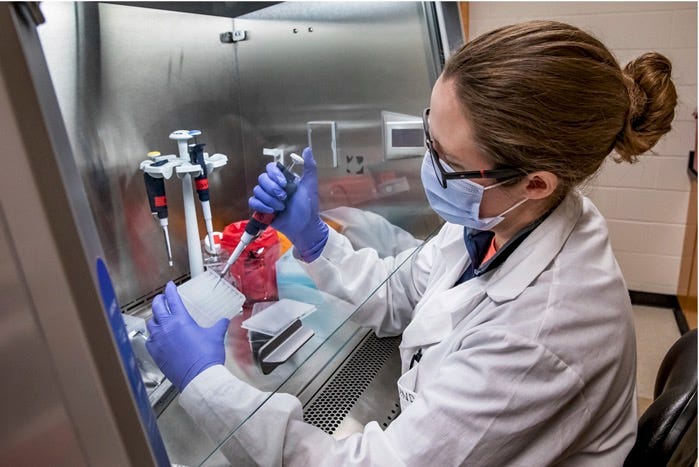
Photo source
Twitter followers know that I’ve long been concerned about the University of Illinois’ SHIELD saliva test. My initial investigation into the school’s claims about having an Emergency Use …
Keep reading with a 7-day free trial
Subscribe to Wood House 76 to keep reading this post and get 7 days of free access to the full post archives.