New York COVID-19 Hospital Frontline: The Silent Witness
An NYC doctor shares what he saw
March 2020 heralded a new heroic figure: the doctor or nurse working on the hospital ‘frontlines’, battling a novel, untreatable and deadly coronavirus. Nowhere did this archetype emerge more suddenly and more prominently than in New York City, the so-called “epicenter” of sudden disease spread in the United States.
Several healthcare-hero archetypes surfaced there in spring of 2020:
The Presumptive Spokespeople like Craig Spencer and Helen Ouyang, providing egocentric, doom-filled descriptions of a crashing, under-prepared system.
The Ostensible Whistle-Blowers like Colleen Smith and Cameron Kyle-Siddell, telling the public about ventilator shortages and misuse.
The Overwhelmed sharing harrowing tales of being besieged by the volume of COVID patients and the severity of their illness.
The Sacrificed – a nurse, ER doctor, or EMT, for example - who reportedly either succumbed to the virus or to the pressures of working under insufferable conditions created by the sudden spread thereof.
The Travel Cadre of nurses and doctors who came on the scene in mid-to-late April to assist, evidently called there by crisis management companies & professional groups. Some recorded tearful videos, later wrote books, and/or established themselves as “early treatment” specialists.
These voices were elevated early in the ‘pandemic’ and, in some cases, their testimonies persist in people’s memories as representative of what occurred.
Yet they comprise a small fraction of the thousands of healthcare workers who were in New York hospitals during the biggest mass fatality event in the city’s history. Most of those thousands are The Silent Witnesses – employees who were on or near the ‘frontlines’ and, to date, have said little to nothing in public about their experiences.
We spoke with one Silent Witness: a radiologist who did not want us to use his name or the names of his employers, but consented to our publishing this article. We call him Pietro.
Some of what Pietro told us during a two-hour conversation in September 2023 complements established narratives, yet he also revealed other things that shed new light or present a new “twist” on what is commonly thought or believed to be necessarily true or representative of what happened on the NYC medical frontlines.
What follows is an account of what Pietro shared, interspersed with relevant data and documentation we have selected to provide context.1
Calm Before the Storm
Pietro was working as a radiologist in two different New York City hospitals when stories about a strange pneumonia in Wuhan, China, surfaced. Hospital and other officials had been saying winter 2019/20 was a rough flu season and were urging staff to get the flu shot, if they hadn’t already. Despite city data showing emergency department and hospital admissions for influenza like illness (ILI) rivaled the 2018 season, Pietro didn’t recall his hospitals being especially busy.
As officials announced the first “novel coronavirus” cases in the U.S., Pietro said he and his colleagues remained calm. There weren’t an unusually high number of patients in February, as far as he could remember, nor did he notice patients presenting with unusual symptoms or chest x-rays.
No one was “taking Covid too seriously,” he said.
The Fallout
After a healthcare worker returning to New York from Iran tested positive, providing the city’s first confirmed Covid case, the tension in Pietro’s hospitals began to build. The “fallout,” he called it, cascaded during the first weeks of March 2020, as federal, state, and local updates on new cases became more frequent and intense.
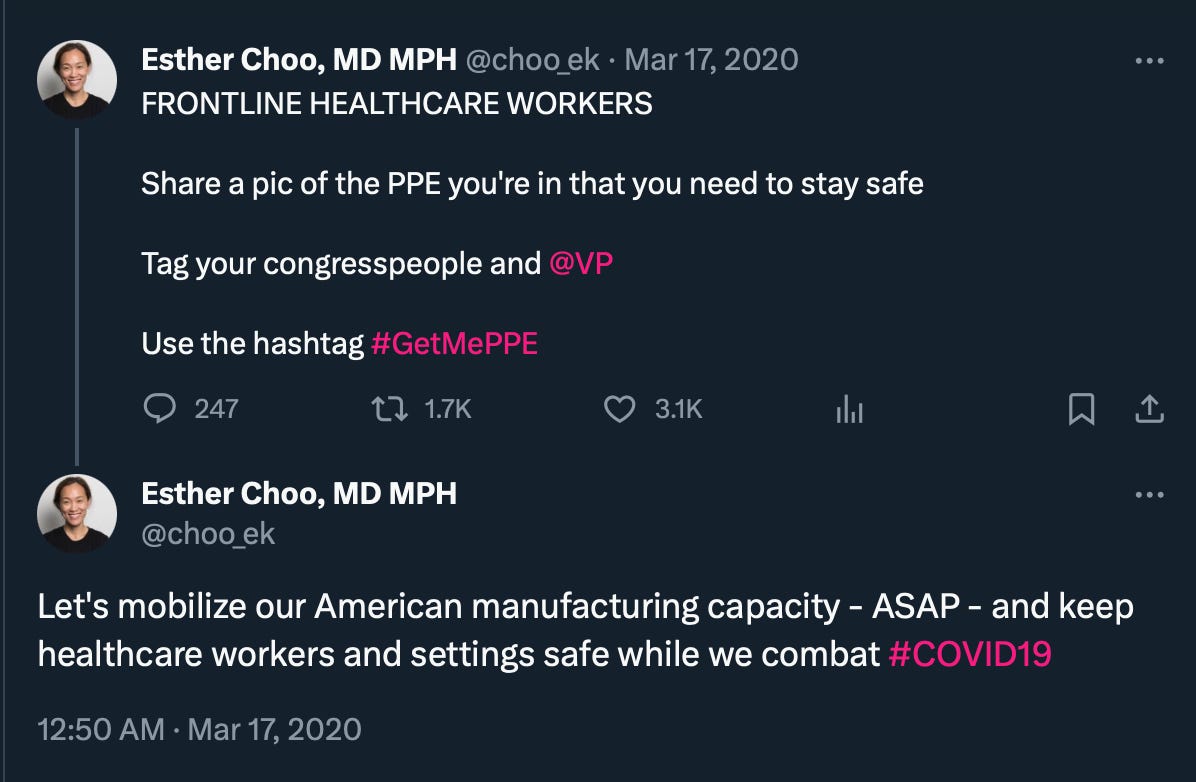
“Staff were panicking,” Pietro said, with some colleagues stealing PPE from the hospitals. The New York Times reported such theft in a March 19, 2020, story - albeit at a hospital in Washington, D.C.2 Scarcity was suddenly a resounding theme – not enough staff, not enough beds, not enough oxygen tanks or masks, gowns, & gloves.3
Pietro was dismayed by some of his colleagues’ reactions, which he felt ran contrary to the fundamental requirement of a healthcare worker’s job: to remain calm, especially during a crisis, for the benefit of the patients.
Looking back at alerts and announcements from health agencies and hospital systems, it’s easy to see why some staff were afraid. Messages went very quickly from promoting calm to pushing panic.4 Organizations such as the American Medical Association and consulting firms like McKinsey told hospital administrators and doctors that difficult decisions would have to be made about resource allocation and would impact decision making about who should live or die. Social media posts reported a “deluge” of patients. Elected officials yelled about ventilators as necessary weapons. Governor Cuomo and Mayor DeBlasio called for military assistance.
Amidst the cacophony, Pietro witnessed many of his colleagues succumbing to fear and inexcusably abandoning their posts during what they were told was a war.
We were left with the impression that actions taken by hospital management were akin to a general allowing the propagation of rumors damaging to troop morale and encouraging desertion — the very opposite of what effective leadership should do in a crisis.
The Tents: Keep Out?
On March 15, 2020, the NYC Department of Health announced “widespread community transmission” of the novel coronavirus.
Pietro’s hospitals - like many others across the city – set up tents, for triaging and testing Covid patients, outside the building.5
Testing/triage tent at Jacobi Medical Center on March 26, 2020. There is no line of patients outside of the tent. Photo taken by a NYC Health + Hospital employee and used with permission.
Pietro and his colleagues expected they would soon see an onslaught of people rushing to the hospital with illness. There was a brief influx of people coming to his who were first handled in the tent, which was less like a barrage of suddenly-sick patients than it was a sudden surge of worried well. It seems to us the real impact, if not the purpose, of the tents may have been in the messages they sent to staff, media, and the general public. An unprecedented disease emergency exists! Hospital intake must be protected! Dangerous virus inside–Keep Out!
Because he didn’t directly attend to patients in the tent, Pietro couldn’t say whether and how people were treated there, or estimate the rate of entry of patients from the tent into the hospital building. He did, however, evaluate, inform, and manage patients in the next stage of triage, in a wing of the emergency department, where he saw a combination of patients with minor symptoms who were concerned about Covid, and some who were sicker, but not necessarily with severe symptoms.
Not everyone coming in the “initial surge” was tested for the coronavirus, he said, unless they met certain criteria.6 Regarding patients who were sent home (versus admitted as inpatients), he speculated that some could have had infections that were incipient pneumonia and weren’t diagnosed or treated, irrespective of the causal agent(s).
On the Inside
Pietro’s descriptions of what he saw deeper inside his hospitals during the frontline weeks support other reports of what was going on, but were also more nuanced. His experiences in the wards was as a clinician, mostly performing minimally invasive procedures for patients.
Premature use of mechanical ventilation. Reports of premature intubation and mechanical ventilation in New York City hospitals were widespread following the first two weeks of “15 Days to Slow the Spread.” A normal pathway for respiratory support would have been nasal oxygen, followed by a bipap machine, and then intubation. Pietro felt some decisions to intubate patients were not being made on empirical grounds or as a result of specific symptoms, but did not observe a high rate of bipap being skipped altogether. “Rarely did I see someone go from nasal cannula to intubation,” he said. “What was more frequent was prematurely advancing a patient from bipap to intubation, in anticipation of deterioration (which was all but guaranteed as a result of the mismanagement).”
Isolation. To further reduce the chance of infection, staff minimized contact time with and around Covid patients. A 15-minute rule was put into effect, Pietro said, and enforced via constant time monitoring and reminders from other doctors and nurses to not stay in a patient’s room too long. As a result many patients and their rooms were not adequately cleaned.
Poor arterial line management. It was in patients’ rooms that Pietro observed poor arterial line management. He reported high incidence of septicemia, clot formation in the line, and vasculopathy, exacerbated by patients not being well-hydrated or adequately anticoagulated.
Interestingly, Pietro also made some observations that are a little surprising in light of other official data and reports:
Younger adults in the hospitals. Despite official data that show an inordinate number of younger adults dying as New York City hospital inpatients, Pietro did not observe young people being hospitalized with Covid or being intubated. Most patients were elderly and chronically or critically ill.
Morgue trailers. Officials announced on March 25, 2020 that the city had purchased 45 refrigerators trailers - formally known as Body Collection Points (BCPs) - to place near hospitals, in anticipation of overflow from hospital morgues. These units were widely featured in media at the time, effectively proffered as evidence that a mass fatality event was occurring or would soon occur.7 As to his own encounters with the trailers, Pietro said, “I saw trucks outside in the back of the hospital that I was told were for the morgue, but didn't see anything other than that.”
Image from “People Are Dying: 72 Hours Inside a Hospital Battling Coronavirus” (March 25, 2020, The New York Times)
The ‘Secret’ Covid ICU Ward
Perhaps the most perplexing part of what Pietro described to us was a ‘secret’ Covid ICU ward located in another wing of one of his hospitals. When he first became aware of the ward, he asked a colleague what was going on there and received the response: “You don’t want to know.”
Pietro ended up being in the ward, doing the same kinds of minimally-invasive procedures he was doing elsewhere. He noticed that many who were staffing the ward were not hospital employees. Under their PPE, uniforms suggested they were military personnel. Pietro referred to some as “Naval Health Officers” and said they interacted with him in an “inquisitive” way and with a “deferential” manner - as though they valued and perhaps needed his input, because they didn’t have relevant expertise.
Real-time press releases and news reporting corroborate Pietro’s account, insofar as military presence in NYC hospitals is concerned. The federal government apparently sent 291 military medical personnel to NYC Health+ Hospitals, the public hospital system. Whether and how that relates to the National Guard pararescuemen mission in Elmhurst Hospital or activities undertaken by staff from the USNS Comfort who were moved ashore isn’t clear.
Covid: A Novel Illness?
Throughout our conversation, Pietro expressed doubts about the novelty of Covid. Because he was working as a hospital radiologist in spring 2020, Pietro was able to describe what he was seeing in the lungs of Covid patients. Of the “ground-glass opacities”, initially widely reported as uniquely symptomatic of Covid, Pietro said such patterns are “pretty common” symptoms of many other pneumonias. “I don’t think there are unique signatures,” he said, later clarifying, “Radiographically, Covid pneumonia isn't something unique - there are other disease processes which look very similar on imaging.”
Pietro’s experiences in 2020 and thereafter seemed to raise more questions for him than answers. “What is this Covid?” he wondered aloud. “What is this novel thing?“ He didn’t doubt the existence of SARS-CoV-2, but he expressed doubts about how the presence of viruses during episodes of respiratory illness relates to or necessarily causes that illness.
Did Pietro think a serious illness of a novel kind “hit” New York in spring 2020?
He didn’t know. But, having lived in New York City he had a keen sense of how little it takes for an already-sick, vulnerable, and government-dependent population in a large and dense metropolis to be adversely affected by sudden changes.
He noted that even minor disruptions in different systems that keep the city’s economy, healthcare, and other functions going in normal times can have significant adverse impacts. He cited a good example of this: trash pick-up was cut back during the spring emergency period and as a result the waste piled-up in many densely populated neighborhoods and this might make more people sick.
Pietro also pointed out that people who live in a large city, whether by choice or circumstance, rely heavily on many government services for their day-to-day existence. For that reason alone, they are generally more likely to listen to what the government tells them to fear – and to expect governing authorities to keep them safe. This meant that the old and the vulnerable readily followed government diktats to isolate themselves and hospital staff obeyed agency & health system directives without hesitation.
Exactly what New Yorkers were being kept safe from in March 2020, Pietro still wasn’t sure.
Breaking the Silence
Pietro’s testimony provides a first-hand report different from the “Healthcare Hero” storylines which emerged during and subsequent to the spring 2020 New York City mass fatality event. His perspective suggests NYC hospitals were not initially fearful about the prospect of the Wuhan coronavirus arriving in the USA. It took administrative fear-mongering to transform staff mindset and behavior from calm to alarm.
It seems a “switch” flipped very quickly and in opposition to what anyone might reasonably expect from hospital leadership in a crisis (especially in a city with more emergency preparedness experience than anyplace else in the world). Multiple agencies, from health authorities to management consultants, told hospital staff they were in a war situation without the proper protective equipment, facing a novel and deadly pathogen. This is a recipe for disaster. Furthermore, pushing the idea that the virus is highly transmissible, and enacting new policies that excused staff’s fears and perceptions of risk — and prioritized those over the care of patients — was unethical and lethal.
As a result, long established day-to-day health protocols and routines were severely disrupted. Patients were prematurely rushed to ventilation. Arterial lines were often not cleaned, increasing the risk of sepsis and other infections. Patients were not properly monitored and were isolated with minimal care and contact, giving rise to more infection risk and psychological trauma and despair.
The fact that the critical care patients Pietro saw were the old and infirm, rather than the young, suggests the spring 2020 death wave affected exactly the same cohort we would expect to suffer from any other ILI. In this sense, it wasn’t novel. Nor did Pietro see “Covid pneumonia” as a unique or remarkable form of pneumonia that could not have resulted from another disease progression or cause.
How do we reconcile Pietro’s experience with New York City hospitals reporting a massive increase in younger adult inpatient deaths in those weeks, with the bulk blaming COVID-19 as underlying cause?8 One possibility is he simply didn’t encounter such patients or such patients were more prevalent at other hospitals.
The same logic may apply to explaining why Pietro couldn’t confirm the presence of morgue trailers per se or see an unusual number of trucks. He simply didn’t encounter them or they weren’t a part of the landscape in his hospitals during those weeks.
Together, all of these contradictions have left Pietro, and us, asking fundamental questions about what happened on the NYC hospital frontlines, and whether the death and disruption in spring 2020 might not have been caused by a sudden-spreading novel pathogen, but rather by the sudden activation of disaster-response plans.
We offer Pietro’s story not as a definitive version of the truth, but as a call for similarly-situated New York City doctors and nurses to break their silence and share what they saw.
Thanks to The Daily Sceptic for mentioning our article in its December 17, 2023 News Round-Up
Access all posts related to my ongoing New York City Spring 2020 Inquiry at the page below.
The unrecorded conversation took place via Zoom over approximately two hours, with no condition or expectation of using the material for publication. Pietro also provided us with additional information and clarifications in follow-up correspondence.
“The George Washington University Hospital in Washington, D.C., has told healthcare workers they can use a respirator mask five times before discarding it, and it is keeping its supply of masks under lock and key. ‘We’ve experienced outright theft, with the general public walking into our building and walking right out,’ said Bruno Petinaux, the hospital’s chief medical officer.” https://www.nytimes.com/2020/03/19/health/coronavirus-masks-shortage.html
For examples, see the NYC health department’s Health Alerts from February 2020 through April 2020 and emails from a surgery department chair in a private hospital system.
This is consistent with CDC guidance around this time.
President Donald Trump talked about images of body bags and trailers at Elmhurst Hospital (Queens) in a March 30, 2020 press conference. The following day, The Wall Street Journal said Trump “ultimately” extended social distancing directives through April 2020 because, according to aides, “he was convinced by the numbers and reports about refrigerator trucks being used to hold the bodies of people who have died of the virus at Elmhurst Hospital in New York City.”
See Figure 14. COVID-19 is U07.1 in the WHO ICD-10.













Hopefully as more 'silent witnesses' begin speaking, it will be easier for the others to come forward....
This reminded me of something out of The X-Files or something.
I know this sounds crazy. But this felt like a trial run for whatever they're going to do to us this election year. It's horrifying. Thank you for staying on it. Please never give up. The more time passes, the harder it is to get accurate information.