Pierre Kory’s New York Story
Observations and questions for a doctor who arrived after The Main Hospital Death Event
In recent weeks,
& I have engaged in debate with regarding characteristics and manifestations of COVID-19.1Despite being a relatively prominent American figure in the COVID Era, Dr. Kory is not someone I recall being familiar or engaging with on Twitter before 2023. After my suspended account was restored, I became more aware of his story, as a part of my ongoing interest in the New York City spring 2020 mass casualty event.
Kory is a New York native who was living and working in Wisconsin when the WHO declared a coronavirus pandemic. In late April 2020, he was among the many out-of-state healthcare workers who traveled to “the epicenter” to work in hospitals.
Unfortunately, official data related to the New York City’s staggering city death toll appear false. Authorities have not yet disclosed proof the event occurred as presented. There is no complete list of names, no way to obtain death certificates of all the deceased, no federal inquiry into what happened or why, and very little interest from American anti-mandate/health freedom advocates in probing what transpired.
The unbelievable hospital mortality is not well- or fully-explained by ventilator use, extant data on nursing home residents who died in the hospital, or Remdesivir. We also have bizarre death processing reported by the medical examiner, and a taxpayer-funded hospital system refusing to release basic data to the public.
Like Pietro, an anonymous doctor we interviewed, I believe Pierre Kory’s experience in New York is an asset to exposing the truth about the New York event. In this post, I present observations and questions about things he has said or that have been documented about what he saw and did in the first half of 2020.
My aim is not to discredit Pierre Kory, nor to challenge his claim that he is anything other than a caring professional who did his best by the medical residents and patients he attended. His advocacy for Ivermectin and against the COVID shot are well-known and appreciated by many, but are beyond the scope of this post and my study of the New York event.2
A delimited timeline and sources of interest follows:
October 2019 - April 2020 — Working in University of Wisconsin Hospital and Clinics, Madison, WI (Critical Care Service Chief, Medical Director, Trauma and Life Support Center)3
March/April 2020 – Involved in the formation of Frontline COVID-19 Critical Care Consortium (FLCCC).
April 6, 2020 — Quoted in press release about COVID-19 treatment protocols.
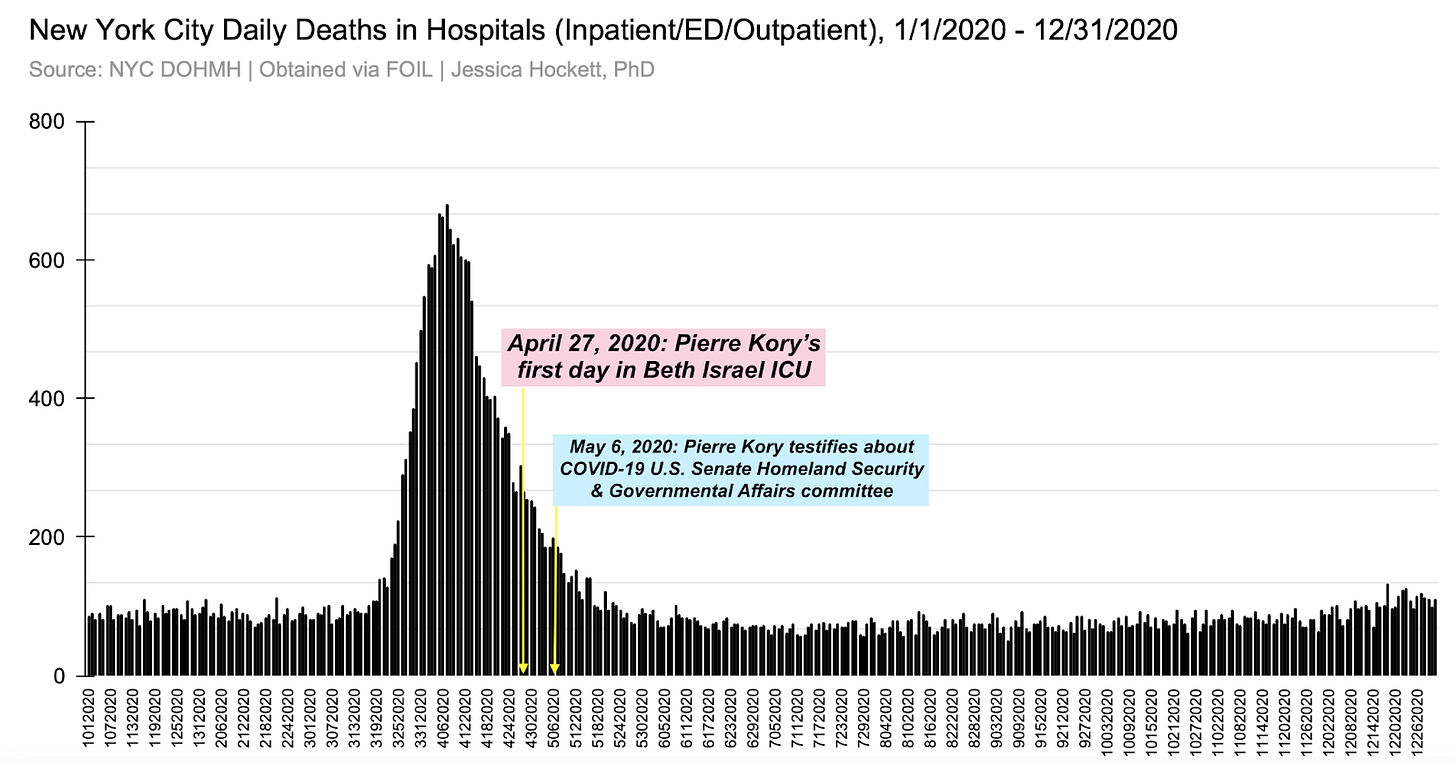
April 27, 2020 – First day in Mount Sinai Beth Israel Hospital, NYC, COVID-19 Emergency Critical Care Attending.
May 6, 2020 – Testified as one of six witnesses at COVID-19 Roundtable, US Senate Homeland Security Committee
July 1, 2020 — Published op-ed in USA Today with Dr. Paul Mayo, “ICU Doctors: Many More
August 8, 2020 — Interviewed by Sean Burke, coinciding with New York Times article “The COVID Drug Wars that Pitted Doctor vs. Doctor”, which spotlighted Kory and others.
I present my observations and questions in categories:
A. Before the Federal Emergency
B. During the Spring 2020 Federal Emergency: UW Hospitals
C. During the Spring 2020 Federal Emergency: Leaving for New York City
D. During the Spring 2020 Federal Emergency: In New York City
E. Witness at U.S. Senate Homeland Security & Governmental Affairs Committee Roundtable
F. Interview on The Sean Burke Show
G. Younger-Adult Deaths in New York City
H. A Non-Coronavirus Explanation?
All of the figures I reference are at the end of the post.
I invite Dr. Kory’s responses, corrections, and clarifications and would welcome the opportunity for a face-to-face conversation.
A. Before the Federal Emergency
In fall 2019 and the first four months of 2020, you were working for University of Wisconsin Hospital and Clinics. Presumably, this means you were seeing patients. Was the 2019 flu season you observed more severe or markedly different than prior flu seasons? Do you recall patients presenting with symptoms or conditions that, in retrospect, you believe could have been “missed” SARS-CoV-2 infection?
Clusters of EVALI cases were reported in Wisconsin in 2019. Did you treat any patients of any age in 2019 with symptoms resembling contemporaneous or subsequent case descriptions of EVALI?
What/whose guidance were you following for “preparing” the hospital for COVID-19 patients (as you mentioned doing in an August 2020 interview with Sean Burke)? Were any existing patients moved into these ICUs, either before or after being tested?
B. During the Spring 2020 Federal Emergency: UW Hospitals
You told a U.S. Senate committee that, in Madison, you “frantically prepared for the expected surge of patients.” Why was a surge expected?
In August 2020, you told Sean Burke, “I was chief of the critical care service and medical director of the main ICU at University of Wisconsin. And we were preparing like crazy for it to hit Wisconsin. Remember, there was a huge delay before you started seeing any– so I was really busy at work, helping teams prepare. We were almost re-inventing the hospital and workflows and processes.” Was there a surge?
At what point in time did you begin seeing new patients coming into the UW hospital presenting with symptoms that were new or unusual? What were the demographics of these patients? Did you get a sense of who they were and where they came from?
When did COVID testing begin at UW? Were all existing patients tested? Do you recall which/whose tests were being used?
Were all patients who were admitted to the ED and/or as inpatients to the hospital in March and April tested for COVID-19?
Your description of the early weeks in Madison says you led daily COVID briefings at UW, “attended in person and remotely by all residents, hospitalists, and intensivists in charge of taking care of COVID patients.” Did you attend to COVID patients as well?
You told Sean Burke you left for New York “once it seemed that the curve flattened in Wisconsin.” Whence the patients during the surge? Were they transferred from nursing homes? Moved from within the hospital to COVID wards? When did the surge end? Did you have a sense of why it ended? (What ended it?)
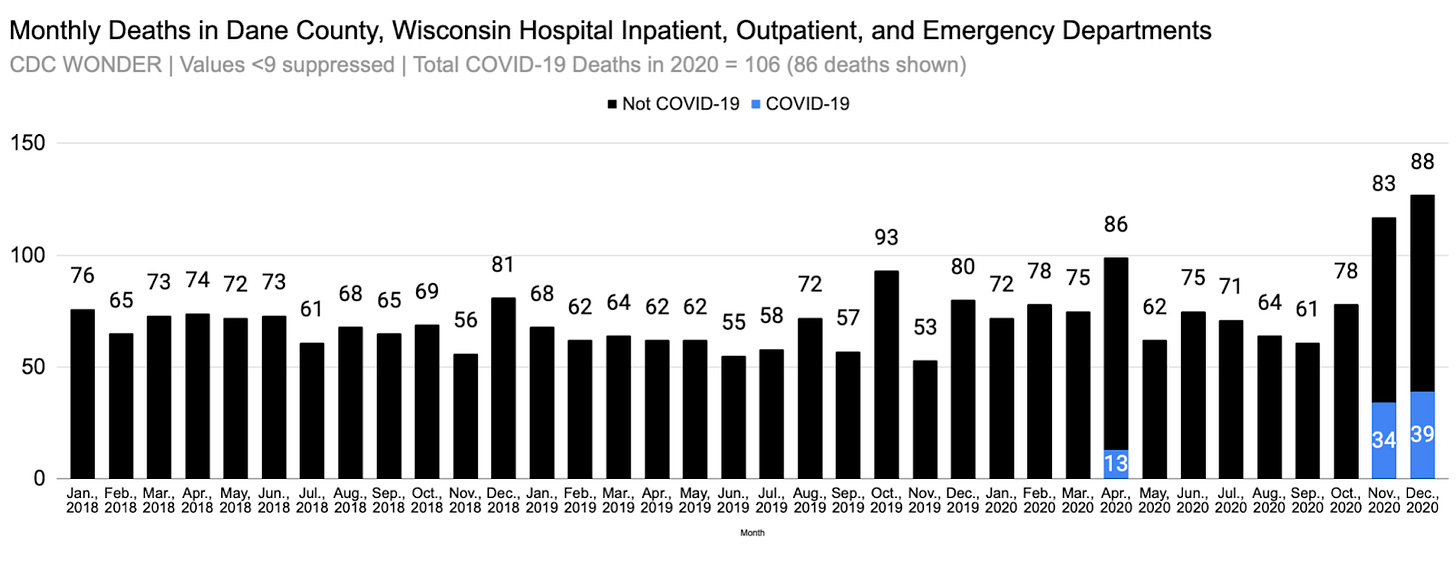
Federal data show that Dane County, Wisconsin, did not experience a significant increase in hospital deaths in spring 2020 – or a high number of COVID-19 deaths (figure 1). Do you recall how many deaths you observed that attributed COVID-19 as the underlying cause?
You’ve suggested that a push for “early intubation” at UW came from other doctors who were scared. Were they scared because of what they were seeing clinically? How many doctors comprised (what you called) “the early intubation crowd”? How long did this early intubation last before [your words, “my colleagues and trainees carefully listened and for maybe the first and last time in the pandemic, simply trusted my judgement” and ceased the approach they were using?
An April 6, 2020 FLCCC press release says, “If you can administer ascorbic acid and corticosteroids intravenously starting in the Emergency Room and every 6 hours thereafter while in the hospital, the mortality rate of this disease and the need for mechanical ventilators will likely be greatly reduced,” says Dr. Pierre Kory, the Medical Director of the Trauma and Life Support Center and Chief of the Critical Care Service at the University of Wisconsin in Madison. He explains that it is the severe inflammation sparked by the Coronavirus, not the virus itself, that kills patients. Inflammation causes a new variety of Acute Respiratory Distress Syndrome (ARDS), which damages the lungs. Should this be taken to mean you were successfully using these treatments with patients at UW?
You’ve said on multiple occasions that you were in touch almost every day with ICU Directors in New York. How did their reports compare to what you were seeing in Madison? Did you report to those doctors what you and your colleagues were and weren’t seeing?
C. During the Spring 2020 Federal Emergency: Leaving for New York City
Regarding what prompted you to go to New York, you’ve said in various forums that you felt compelled to go help former colleagues and have referred as well to email lists of professional organizations. For example, you said [via Substack comment], “The Chiefs of critical care in NYC were sending out, via society email lists, ‘Intensivists Needed in NYC Now,” and that you showed up in New York in response to that call. Do you have examples of those solicitations? (They would be helpful to see, for archival/historical purposes re: the non-military “travel cadres” that descended on the city.) Were there people or factors that influenced your decision to go to New York, or was it largely those email lists?
You told Sean Burke you left UW for New York on a Humanitarian Leave. Did you have to formally request/apply for the leave? Was anyone not employed by UW involved with initiating or approving the leave?
Senator Ron Johnson (R-WI) was your senator at the time. Did you and the Senator or the Senator’s staff communicate in late 2019 or the first months of 2020, prior to you leaving for New York City? Had you ever met the Senator (either virtually or in person) before 2020?
D. During the Spring 2020 Federal Emergency: In New York City
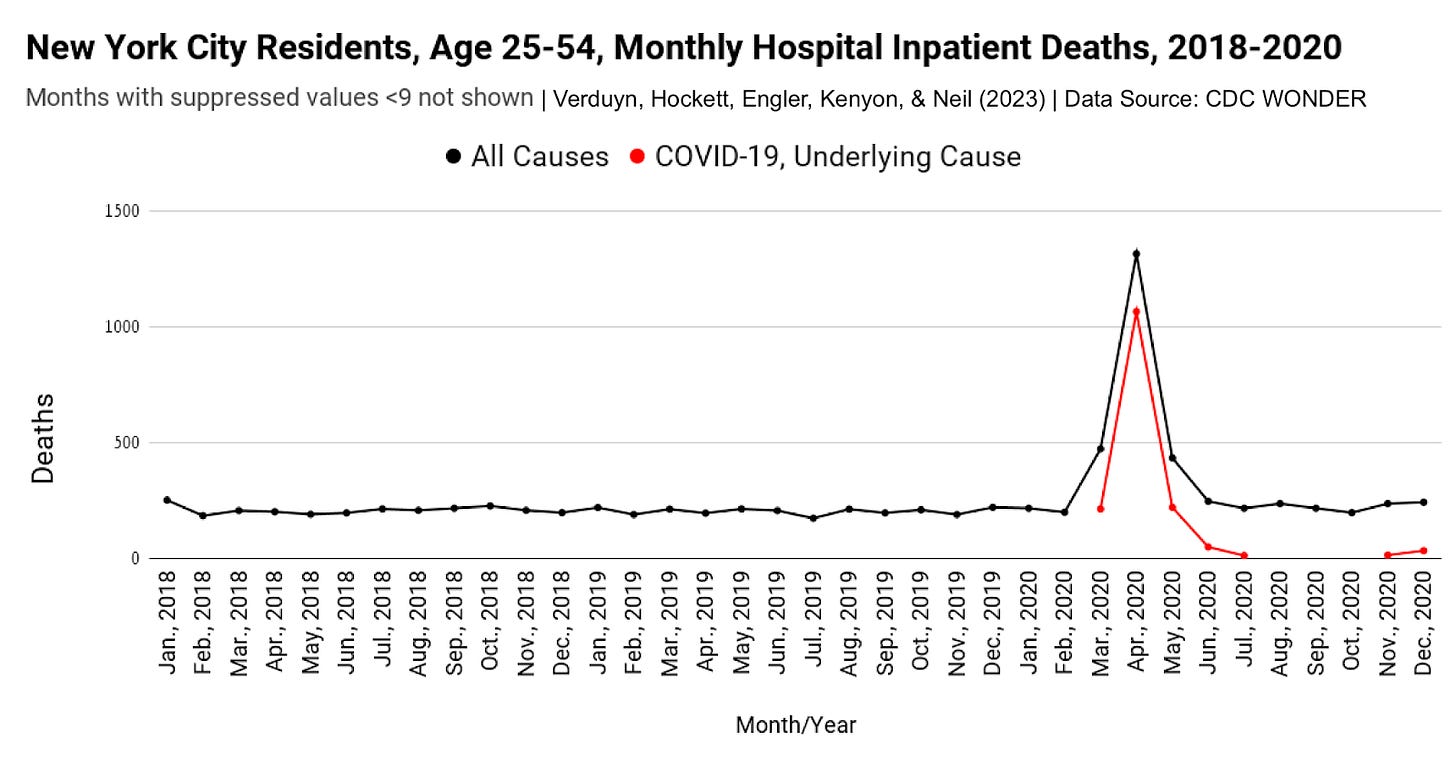
You’ve said your first day in the Beth Israel ICU was April 27, 2020. This was after the main death event, per federal data (figure 2). Does this data surprise you, or does it seem consistent with what you witnessed in the timeframe?
What was your date of arrival in New York City? Did you go to other hospitals, either before you started at Beth Israel or during your time in the city, whether in the five boroughs or metro area?
You’ve said that you took over your “old ICU,” which was 16 beds, all filled with patients on ventilators with COVID, many of whom had been on vents for weeks. Although intubation data are incomplete and insufficient, what you’re saying fits with the state’s file, which shows a sharp rise in patients intubated, followed by a long, slow decline. Did you get a sense of who these patients were and what they were admitted for? Did those 16 patients die? Are they examples of patients who were “actively dying” - a term you’ve used to describe deteriorating patients who become “irrecoverable”?
You’ve written about the number and nature of conversations that you had with families in New York regarding end-of-life care and decision-making. Did your hospital allow family members to visit their loved ones in the ICU? Did the conversations you reference take place in person over the phone/via Internet? Did you witness DNR orders being given for COVID patients - unilaterally, without third-party witnesses?
You’ve described being in a COVID ICU you were “leading,” with patients whose chest x-rays and presentation all looked the same.4 You’ve also said there were multiple COVID ICUs – which is consistent with descriptions of how hospitals “rearranged” in preparation for the so-called COVID surge. According to your CV, you were the director of simulation training at Beth Israel from 2008-2015 and COVID-19 Emergency Critical Care Attending in May 2020 at Beth Israel (which implies that you were overseeing residents). Such details are relevant to the theory that NYC hospitals ran a live-exercise simulation in those “surge” and post surge weeks. Do you think it’s possible that you (and others) may have been called in to follow up on or help oversee/evaluate the later stages of a simulation — one with live patients? Have you considered the possibility that NYC hospitals “ran” a live-exercise of some kind, to simulate disease spread, unbeknownst to most staff, including yourself?
Officials, media reports, and healthcare worker stories indicate there was military presence in at least some NYC hospitals. Did you encounter military personnel (e.g., National Guard, Naval Health Officers) at Beth Israel? If so, did you speak or interact with any, and do you know why they were there and what they were doing?
On what day did you depart New York? What was the official reason for your departure? (Your CV indicates you were there for five weeks; elsewhere you’ve said four weeks. The use of present tense in the opening sentence in your 7/1/2020 USA Today op-ed with Dr. Paul Mayo indicates you were still there.)
There is some confusing language in a New York Times August 8, 2020 article regarding when you left UW. In an interview with Sean Burke on the same day, you seemed to suggest your resignation was in May. Can you clarify?
E. Witness at May 6, 2020 U.S. Senate Homeland Security & Governmental Affairs Committee Roundtable - COVID-19: How New Information Should Drive Policy
When did you receive a request to testify at the May 6, 2020 meeting? When did you accept the request?
Were you given guidelines or parameters for your testimony, either in writing or via other communication?
Especially given your relatively late and then-very-recent arrival in New York City – the site of an incredible hospital mass casualty event – it’s curious that the Senate committee did not call a witness who had been in hospitals since February or March, at least. Do you know if other New York City doctors or administrators were asked to testify at the May 6, 2020 roundtable?
Introducing you at the May 6, 2020 meeting, Sen. Johnson said, “I just spoke with him last week,” which would have been sometime between April 26 and May 2, 2020. Was that the first time you ever had direct contact with Senator Johnson?
You told the committee, ”The mortality and morbidity rates of this disease are unprecedented. I’ve been doing critical care for a decade and a half. I do not see mortality rates associated with any severe illness that I see in this one.” This was a very bold statement, even at the time — one that gives an impression of a very deadly illness which does not seem to have been observed in most places in the U.S. and around the world, including Chicago, which reported a first case six weeks prior to New York. Have you considered whether what you were seeing or your perception thereof was influenced by factors that didn’t involve a spreading flu-like pathogen?
You told the committee, “Either I’ve been inundated with patients who are chronically on the vent who are dying of end-stage fibrotic lung disease, or I’m seeing patients who are crashing into my ICU, but as opposed to a month ago, where they were coming in with these mild abnormalities on chest x-rays and maybe mild abnormalities in their oxygen intake. Now, we’re seeing floridly abnormal x-rays, with very advanced disease.” You were not in the Beth Israel ICU “a month ago” (April 6, 2020), correct? Was this comparison based on what other employees of the hospital told you they witnessed? Who were these patients? Did you get a sense of their past medical history?
You told the committee, “I’m throwing the book at ‘em, and it’s not working. I have to emphasize that the timing of the initiation of this therapy is critical. The world needs to know this.” What specific therapies were you using that weren’t working?
You told the committee, “What happened here in New York is that the initial surge caused so many terrible reports of patients being unattended to, running out of resources, not enough physicians and nurses.” Who was supplying these "terrible reports"?
You went on to say, “They’re not coming to the hospital early enough. Now when they’re coming — they’re so far advanced that the medicines don’t work as well. And so we need to get the word out that things are better on the ground. We’re definitely much more stable in the hospitals. We’re much more resourced. We’re re-grouped. We’re ready to take care of patients, but the patients have to come. If they wait at home with these symptoms, we’re not going to be able to save them.” Who were the patients that were coming to the hospital but not early enough? From where were they coming (e.g., private residences, nursing homes, public housing) and how old were they?
In written testimony to the committee, you endorsed the use of Remdesivir as a potential outpatient treatment for COVID, stating, This is the phase anti-viral therapies should be focused on, i.e. before patients reach the hospital where medicines like hydroxychloroquine or Remdesivir would have the greatest impact to keep the patient away from the hospital and ICU, p 5). Did you administer, oversee the administration of, or have knowledge about the drug being used at Beth Israel?
Are your spoken and written testimonies to the committee inclusive and representative of COVID patients you saw in both Madison and New York City?
F. Interview on the The Sean Burke Show, August 8, 2020
You indicated you were using the MATH+ protocol with patients in New York, with little success, which you attributed to your late arrival. (Excerpt below.) Is it possible that the patients you saw – presumably patients who had tested positive for SARS-CoV-2 – were chronically ill patients that were transferred from nursing homes and elsewhere in the hospital and were not suffering from a new disease per se?
Burke : Were you using MATH+ there [in New York]?
Kory: I was. I was using some forms of it. I was getting pushback on some of the Vitamin D, just little [ticky stacks?], but mostly I was using pretty aggressive anticoagulation and methylpred., as well as ascorbic acid. So, yeah actually, I was using MATH, the plus a little bit less so. But certainly MATH was standard for me.
Burke: And the results that you were seeing?
Kory: Well, not the same as my colleagues and there’s some really important reasons for that. And you even mentioned in your introduction is that, you know, especially in critical illness, we talk about this concept of the Golden Hour, or the Golden Hours, which is, when you intervene, before someone goes into multi-organ failure or severe organ failure, you gotta get to them early. The medicines have to be delivered early. And when I got to the ICU on April 27th, many of the patients that I took over had been on ventilators for 1-2 weeks. Some of them had gotten a little bit of steroids not. So I’m going tell you, if you ask me about my results? Not very good. But that’s not to say that the medicine doesn’t work. It was too late. These patients were really, really sick, you know.
Along the same lines, a bit later in the interview you said, “When I was in New York, I saw nothing but - what I would say were patients chronically ill with COVID, I didn’t see acute.” Did you see acutely ill COVID patients in Madison – i.e., patients with sudden onset of respiratory illness?
You also said, “By the time I left New York we had no new cases. So, this is end of May. There was just no new COVIDs that I saw. And since then I’ve been doing research and writing and other stuff.” In retrospect, does it strike you as odd that COVID cases in NYC hospitals simply disappeared in a city of 8.5 million people? Were you aware of any changes to testing protocols or the tests themselves that may have played a role?
G. Younger-Adult Deaths in New York City
You’ve said multiple times you saw younger adults dying of COVID-19 in NYC hospitals. Examples follow:
The severity, morbidity and mortality of COVID-19 must be re-emphasized to all, both young and old, as it spares neither (7/1/2020, USA Today)
I had too many young and healthy (relatively) on vents suddenly - why/how would a bacterial pneumonia suddenly do this unless it was a new superbug which would have been quickly identified (2/23/2023, Substack).
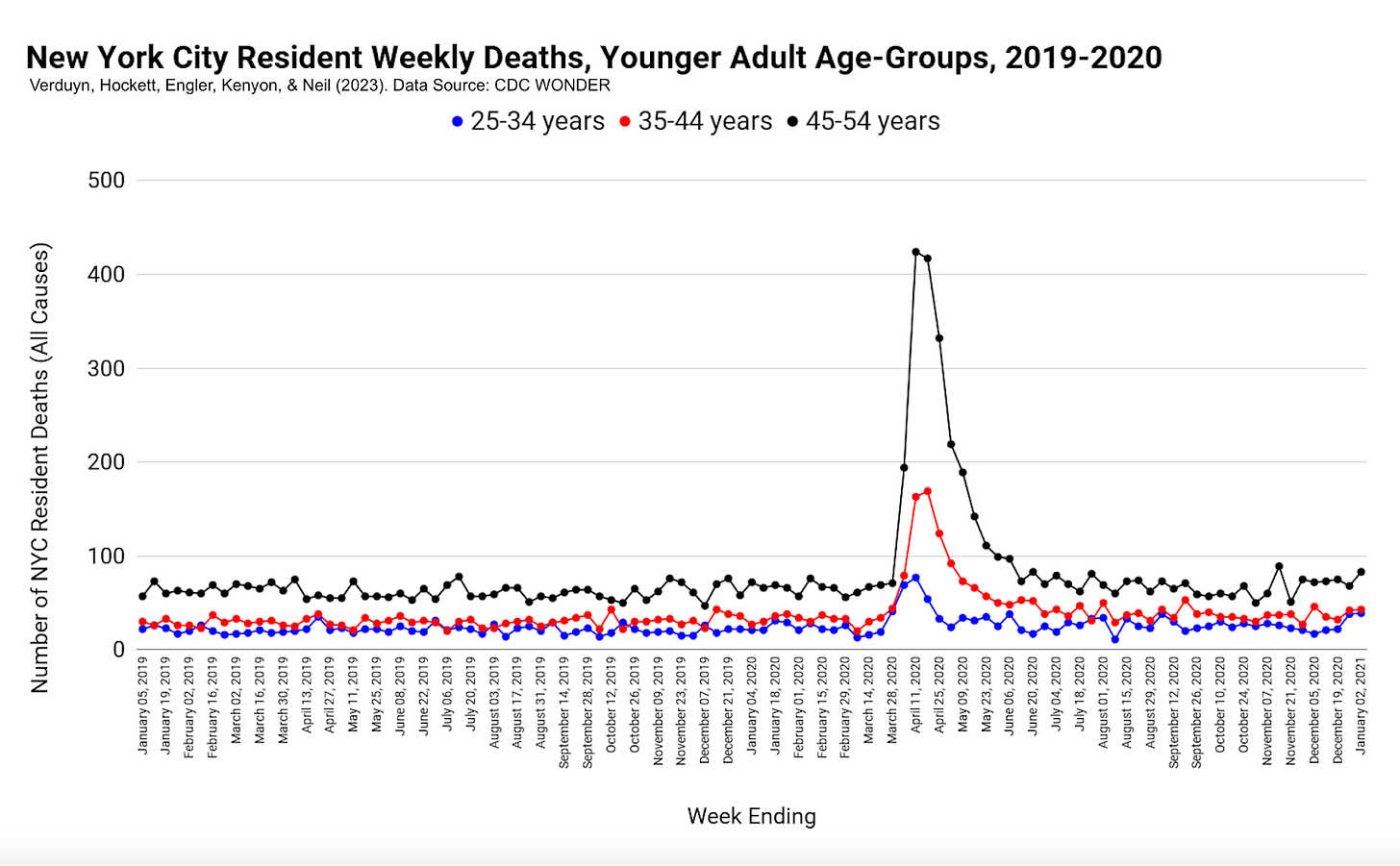
Federal data show steep, simultaneous rises in the number of younger-adult deaths in hospital inpatient (figure 3).
As far as colleagues in PANDA and I have been able to tell, New York City is a global outlier in the speed and magnitude of younger-adult deaths attributed to COVID-19. Nearly all the increase in hospital inpatient deaths among ages 25-54 cites COVID-19 as the underlying cause of death (figure 4).
Do you think a formal inquiry of NYC hospitals is warranted, if only on the basis of the number of COVID deaths among younger adults?
Have you considered the possibility that COVID patient designation, as determined by testing positive, may have led you and other doctors to think it was caused by disease when in truth it was not? For example, people were sick and dying from something else, but being positive on a newly-developed PCR test for a newly-detected pathogen led you to focus on COVID as the main problem?
H. Not a Coronavirus?
Multiple times in 2020 and thereafter, you’ve said that the COVID-19 disease you observed in the first wave of U.S. mortality was very severe and was transmitted from person to person. For example:
At the Senate Committee meeting on May 6 , you painted a picture of a war-zone that is inconsistent with hospital data and with what other doctors in most other cities and countries reported seeing during this timeframe. You said, “We’re at war right now with this virus,” and that “The mortality and morbidity rates of this disease are unprecedented. I’ve been doing critical care for a decade and a half. I do not see mortality rates associated with any severe illness that I see in this one.” Those are very strong words for a flu-like illness. Looking back, how confident are you that you were not observing a scene that was staged or set-up for you?
You and Dr. Mayo said you were “perplexed as to why responsible people would choose not to wear a mask given the potential harm, including death, that they could cause to their fellow citizens.”
In your recent response to Martin Neil, Jonathan Engler, and me you admitted the possibility of "something as preposterous as deliberate widespread release in certain targeted cities and areas."
It seems you may believe there was a point-release of SARS-CoV-2 or another agent or factor at work in NYC. Have you shared your concerns with federal officials? Do you have or are you aware of any specific data to support this hypothesis? If there was such a release, do you think it changes the WHO’s March 11, 2020 pandemic declaration (or your view thereof)?
Finally, do you think your early impressions of the severity and threat of the COVID-19 – and the transmission mechanism – were warranted? If this perception was driven largely by what you observed in New York, have you considered that what you saw has alternate explanations that don’t involve a spreading coronavirus?
2/8/2024 UPDATE: Dr. Kory responded via recorded videos.
Pierre Kory Responds to My Questions About His New York City Experience
Dr. Pierre Kory sent me video-recorded responses to the questions I posed about his spring 2020 experiences in New York City and Madison, Wisconsin. On January 26, 2024, he wrote: Here are my recorded answers to the many questions you posed which was what was requested, I trust it will help you guys in formulating what I think will be a better hypothesis…
Figures
Figure 1
Figure 2
UPDATE, 1/27/23: As the Figure 2 subtitle say, values <9 are suppressed by CDC WONDER database. A query for March and April 2020 combined shows 14 COVID-19 deaths (underlying cause) in hospital inpatient/ED and outpatient. That means 1 such death in March.
Several other Substackers - Sage Hana, Charles Wright, & The Underdog - have also posed questions of Pierre Kory, in their own style, some of which relate to Ivermectin
Via Substack comment: “Beyond PCR tests (which I dont want to get into), is that they presented so similarly, you really did not need a test. Their clinical presentations and CT scans and chest x-rays were identical. I have never in my life run an ICU where I had 24 patients with the same chest x-ray. Literally identical.”


Excellent article, impressive investigative work, and thought-provoking questions!
I just finished listening to the Jimmy Dore and Kory podcast on Rumble, which led to the termination of Mark’s YouTube video from five years ago due to a brief reference. The video included a one-second clip of Dr. Kory, where he dismisses the fentanyl epidemic, noting its absence globally during Spring 2020, when NYC reported 26% of COVID deaths in people under 65. This statistic, both unique and unreplicated since then, seems almost comical.
Regarding Dr. Kory’s comments, I believe they are part of a psychological operation. His assertion that ‘fentanyl has been around for 10 years’ seems like a diversion, and the rest of the podcast appears to divert attention to the topic of vaccine criticism.
This pattern seems recurring among figures like Malone, Bret, and Kory. Initially vocal about ‘worst-case scenarios,’ they now predominantly focus on criticizing vaccines.
Despite the WHO’s declarations, these influencers seem to have played a role in persuading small businesses to shut down and parents to keep children out of school in the name of saving lives, all leading to an inevitable solution: vaccination as a path back to normalcy; But, people who were hesitant to get vaccinated felt pressured, a fact Dr. Kory is aware of. He knows he wasn’t directly responsible for this coercion, so he participates in podcasts as if his conscience is clear. However, I wonder if he harbors any guilt about the outcomes, especially if his initial claims turned out to be untrue.
This appears to be a classic case of a ‘limited hangout’ strategy.
Keep up the great work Jessica! I think, for many of our leaders in the health freedom movement, if the narrative of some sort of pandemic is questioned, their place on the pecking order is lowered. Plus, many really think the only way to nail Fauci & his cohorts is to prove that GOF is an existential threat. I think your work & the work of the HART group is showing that, even if there was a released "deadly" virus that "spread" worldwide, it was pretty much of a nothingburger.